

Surgeons at MUSC use multiple techniques to help children with congenital facial paralysis show their feelings
Victor Borge once said, “A smile is the shortest distance between two people.” But what if one physically cannot smile? The gap widens.
“Facial paralysis can be a very devastating condition,” says Samuel Oyer, M.D., a facial plastic and reconstructive surgeon at MUSC who often works with children. For one of his young patients, he describes that many people in stores or other public places would think she was angry or upset when she was actually trying to smile. This type of misunderstanding can significantly impair positive interactions between people.
Facial paralysis in children is rare but can happen for a variety of reasons. Infections, trauma, tumors and Bell’s palsy can all cause damage to the seventh cranial nerve, which is critical for facial movement, but the cases most commonly seen at MUSC are congenital. And Oyer explains that pinpointing the cause of the paralysis is crucial to determining the correct treatment.
“If it’s an ear infection you treat it with antibiotics and maybe ear tubes. If it’s a trauma or Bell’s palsy you usually wait a little bit and see how much recovery you get,” says Oyer. “But if it’s congenital it’s not going to recover on its own.”
Enter the expertise of Oyer and his surgical partners, Krishna Patel, M.D., Ph.D., and Judith Skoner, M.D., who together run the MUSC facial paralysis clinic, one of just a few such centers in the Southeast. For children with congenital facial paralysis, these physicians offer the chance to learn to smile.
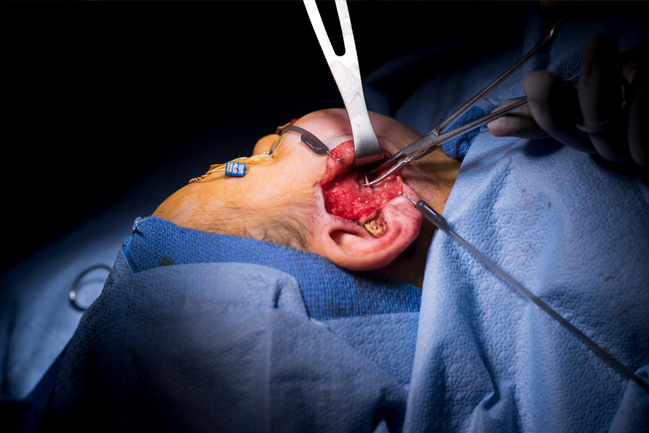 For a patient with a functional masseter nerve, the surgeon reroutes that nerve to a branch of the facial nerve (shown).
For a patient with a functional masseter nerve, the surgeon reroutes that nerve to a branch of the facial nerve (shown).
There are two main surgical approaches to animating a child’s smile. In the first, the surgeon reroutes the child’s masseter nerve to a branch of the facial nerve. Once this nerve detour is up and running, the child can learn to grin by clenching the teeth — the new nerve signal triggers the muscles to lift into a smile.
If the child’s facial nerve can no longer be stimulated to function or never developed properly, the second approach requires a transplant from a leg muscle, usually once the child has reached at least 5 or 6 years of age. This approach involves facial surgery as well as a leg surgery to remove a strip of gracilis muscle along with intact blood vessels and nerves. The muscle is transplanted to the face and attached to the facial blood vessels and a functioning nerve, which may be the masseter nerve or a facial nerve graft from the opposite side. This is performed painstakingly under a microscope to ensure good blood flow and eventual efficient nerve input to the muscle.
Oyer also notes that the art and technique of the muscle placement determine how natural the smile will look. He says, “If one corner of the mouth has a three-millimeter difference in height compared to the other, the eye will pick it up on a glance.”
After several months of tissue healing and waiting for the new nerve to begin firing, patients can start physical therapy to learn to flash their new smile at will.
Sarah Murphy, PT, DPT, works with young facial paralysis patients and their families and is awed by the resilience of these children. “One thing that I think is really wonderful about kids is that they are still so confident,” Murphy says, “No matter what is going on.”
Murphy spends much of her time on parent education, teaching playful techniques so the family can practice together every day. The pediatric facial paralysis team at MUSC sees patients from
across South Carolina and the Southeast, and they are incorporating telemedicine into their follow-up visits to help patients avoid long commutes to the doctor.
Finally, Oyer stresses that for patients with facial paralysis, the sooner the intervention the better. Intervening within less than two years of paralysis onset gives the highest chance of success, but even with an extended timeline or a congenital condition there are options. “We can’t totally recreate what was lost or never formed,” Oyer states. “But we can usually take steps to make it better.”
 A gracilis transplant patient flashes her smile before (left) and after (right) surgery.
A gracilis transplant patient flashes her smile before (left) and after (right) surgery.



